Stimulants, drugs like crack, coke, and meth, are hard on your heart.
Using these drugs can lead to heart disease and overdose.
If you use stimulants bought on the street, or have in the past, here’s what you can do to protect yourself from heart disease and overdose:
Learn the signs and symptoms of heart problems.
Talk to a healthcare provider about getting tested for
heart disease.
Learn what you can do to lower your risk of overdose if you are still using stimulants.

The basics
Stimulants and heart health
Stimulants (or “uppers”) are a class of drugs that speed up the body’s central nervous system. Stimulants exist on a spectrum - from a cup of coffee to a prescription such as Adderall, to street drugs such as cocaine, crack, or meth.
Frequent use of stimulants can lead to addiction. Because these drugs make your heart beat faster and raise your blood pressure, using them at all can lead to heart attacks and using them long-term can wear out your heart — which can lead to heart failure or similar heart diseases.
Overdoses
Philly has seen a big increase in overdose deaths involving stimulants. Stimulant-overdoses are often caused by damage that’s been done to the heart during past stimulant use – which means that long-term stimulant users are at higher risk.
A recent study done by the Philadelphia Department of Public Health found that of the people in Philly who died of an overdose, heart disease was most common among people who died of stimulant-involved overdoses without opioids.
Middle-age Black men in North, West and Southwest Philly are most at risk.
In some parts of Philly, overdose deaths involving stimulants are going up, especially for Black men. From 2019 to 2023, overdose deaths went up 61% among Black people, while they went down for white people.
In 2023, 80% of overdose deaths among Black men involved a stimulant.
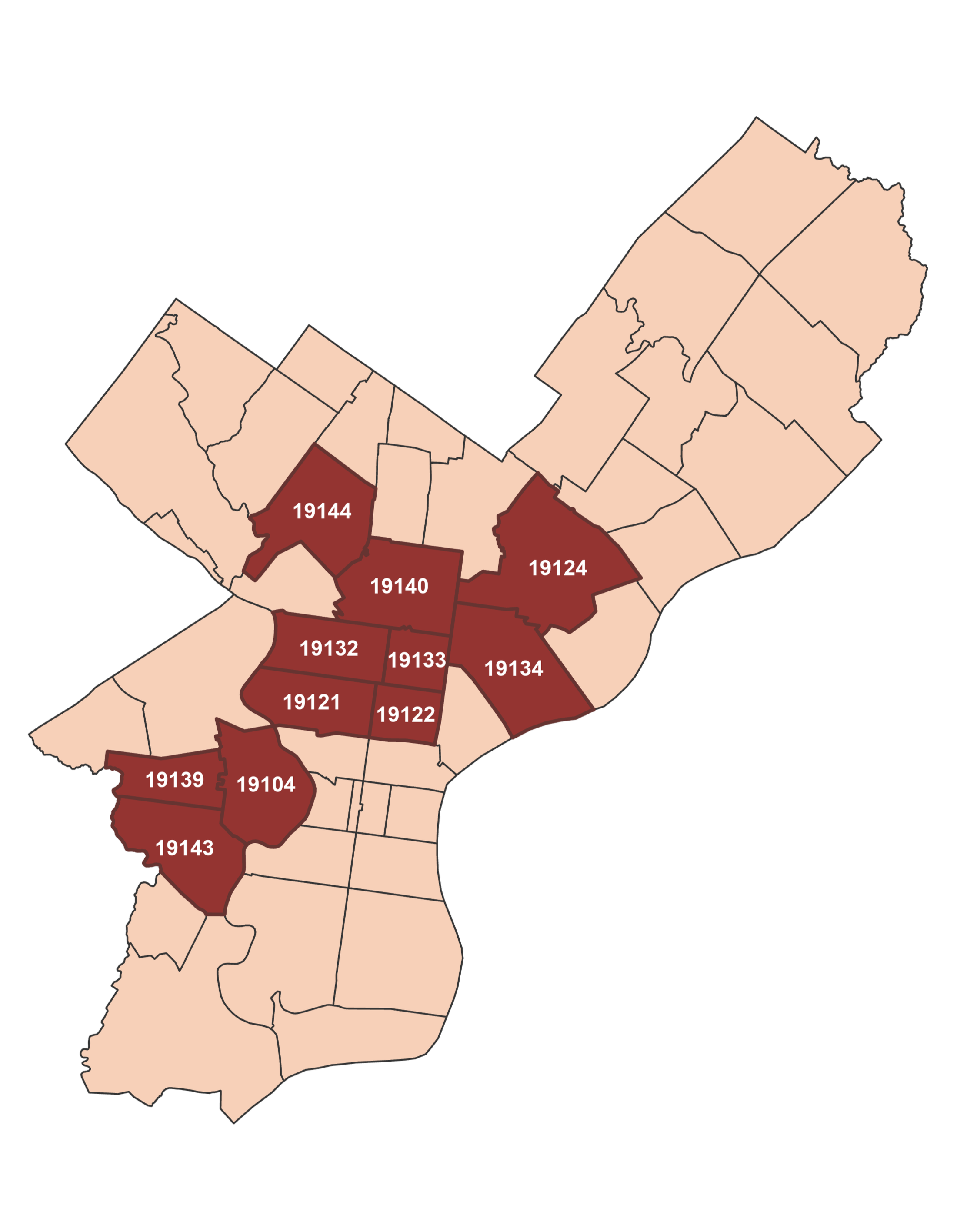
Rates of stimulant-involved overdoses increase most in North, West and Southwest Philly, especially in these neighborhoods:
Cecil B. Moore, Brewerytown
Strawberry Mansion, Allegheny West, Glenwood
Frankfort
Hunting Park, Nicetown-Tioga
Fairhill
East Falls, Germantown
Mantua, Haverford North, East Parkside, West Powelton
Cobbs Creek, Mill Creek
Kingsessing
Elmwood Park
The average age of Black men who died of an overdose in 2023 was 52 years old. This is older than the average age of people who died of an opioid overdose.
Philly ZIP codes with the most stimulant-involved overdoses, 2023

Know the signs of heart disease
Chest pain, tightness, pressure or chest discomfort
Shortness of breath
Pain in the neck, jaw, throat, upper belly or back
Pain, numbness, weakness or coldness in the legs or arms
Dizziness
Fainting or almost fainting
Fluttering in the chest
Racing or slow heartbeat
If you are experiencing one or more of the following symptoms, it is time to see a healthcare provider:

Talk to a doctor
Need to find a doctor in Philly?
Here is a list of clinics with walk-in hours (when you don’t need to make an appointment) for new patients in the ZIP codes most impacted by stimulant overdoses:
Strawberry Mansion, Allegheny West, Glenwood (19132)
East Falls, Germantown (19144)
Cecil B. Moore, Brewerytown (19121)
Cobbs Creek, Mill Creek (19139)
Want to find a clinic closer to home?
Use the City of Philadelphia Primary Care Finder tool to look for a clinic
that meets your needs.
Start the conversation
Talking to a healthcare provider about substance use can be tough - especially if you’ve had bad experiences in the past. SUPHR created a conversation guide to help you talk to your provider about heart health and stimulant use to help you feel more confident and get what you need out of your appointment.
Steps to take:
Describe your concerns about your heart health.
Example: “I used stimulant drugs and want to talk about my risk of heart conditions.”
Describe which stimulant drugs (cocaine, crack, meth) you used, how long, and how frequently.
Example: “I used crack about 3 times a day for the last 10 years.”
Describe any symptoms you have had.
Example 1: “Sometimes, I feel my heart racing and have chest pain.”
Example 2: “I don’t have symptoms, but I’m concerned about my risks.”
Ask questions and describe other concerns.
Example: “Does this mean I have to stop using stimulants completely today?”
Describe what you hope can be done.
Example: “I want to be screened for conditions, like heart disease, that may be related to drug use.”
Print this guide and take it to your appointment with you.

Provider Resources
Stimulants, drugs like crack, cocaine, and meth, are a class of drugs that increase central nervous system activity and levels of dopamine and serotonin in the body. In addition to pulmonary, oral, and infection risks, stimulant use can cause cardiovascular and cerebrovascular conditions. This includes vasoconstriction, vasospasm, increased heart rate, and elevated blood pressure. As a result, people who use stimulants are at greater risk for acute myocardial infarction, stroke, heart failure, arrhythmias, and sudden cardiac death, even among people without a history of heart disease.
In primary care settings, it is essential to conduct blood pressure and heart rhythm screenings for individuals who use stimulants (CDC Stimulant Guide – cite). Dr. Rachael Truchil, MD, MPH, Internal Medicine Physician and Clinical Lead at the Penn Medicine THRIVE Addiction Medicine Clinic, says:
“Traditional cardiac risk calculators do not include stimulant use…I am also more aggressive with blood pressure management in patients who use stimulants because of their long-term risk of cardiac disease. I start talking about hypertension earlier, start medications more quickly, even if patients only have mildly elevated readings, and I treat to lower blood pressure targets.”
Primary care visits are also a good opportunity to discuss a patient’s substance use and how to stop or reduce use. Reduction in stimulant use is often more achievable than total abstinence. Reduced use improves health outcomes for people with stimulant use disorder and should be considered a valid, positive outcome for patients who use stimulants (Aminesmaeili et al.; Coffin et al). Additionally, uncontrolled hypertension and cardiovascular conditions not only lead to more severe health outcomes, but can also have contraindications for some stimulant use disorder medications (START – Boston med 2024).
Not quite ready? We have several resources to make you feel comfortable treating patients who use stimulants. Dr. Truchil’s short video below provides an overview of how she treats people who use stimulants, including indications for cardiovascular screening and follow-up testing. Our division has also created two toolkits to provide clinicians with data on stimulant use, the associated health risks, clinical tools, and resources to use in their practice. The American Society of Addiction Medicine (ASAM) and the Grayken Center for Addiction Training & Technical Assistance at the Boston Medical Center have both developed stimulant use treatment guidance.